
Once a person is transitioned into services, DSPD must determine if the Person qualifies for Medicaid and can be placed on the appropriate Home and Community Based Waiver (HCBW). Determination of eligibility for the HCBW has two main components: Nursing Home or Intermediate Care Facility (ICF) Level of Care eligibility, and Financial eligibility. The Nursing Home/ICF level of care is established by DSPD and managed in the USTEPS system. Financial eligibility is determined by the Department of Workforce Services (DWS). The USTEPS system has the feature to generate the application form for Financial eligibility and the tracking of the determination by DWS.
Level of Care determination is the first step of determining eligibility for Medicaid or the Medicaid Home and Community Based Services (HCBS) Waiver. Level of Care refers to an assessment that indicates that if were not for the option to receive community based services in lieu of institutional services, a Person would qualify for institution based services. DSPD is the Operating Agency for three HCBS Waivers: Community Supports Waiver, Acquired Brain Injury Waiver, and the Physical Disabilities Waiver. The specific requirements for each of these Waivers are discussed later in this manual.
Essentially, if a Person meets the State eligibility criteria, they will also meet the Level of Care criteria for each of the three Medicaid Waivers. This is due to State eligibility criteria being developed and implemented based on the Federal criteria for Level of Care. In this way, conflicts in eligibility have been greatly minimized.
The "Level of Care" screen is found in the USTEPS menu under the Eligibility heading:

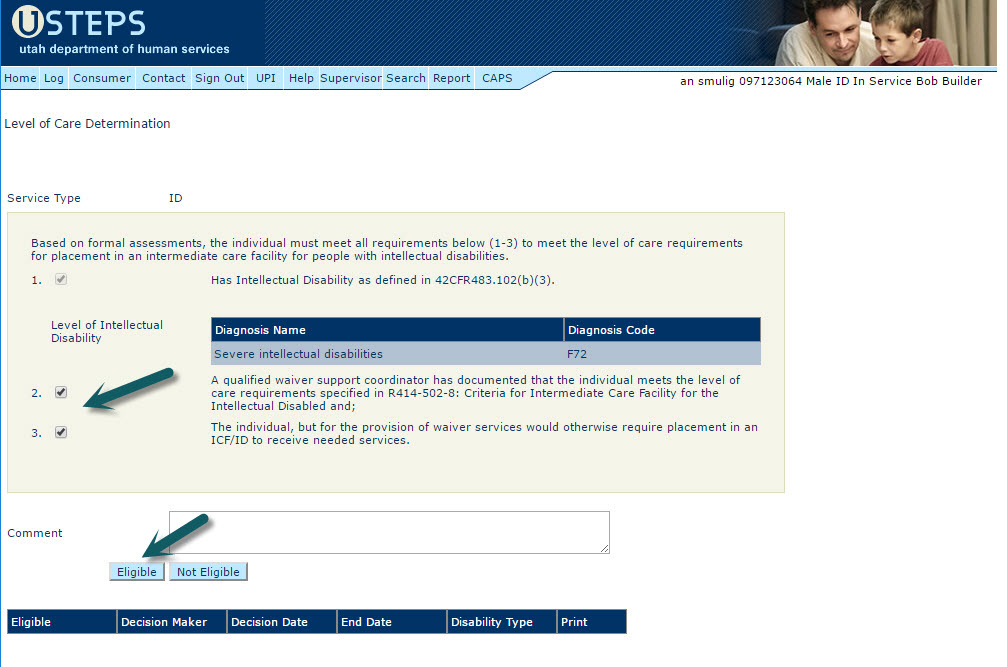
The Level of Care screen matching the Person's disability type will be displayed. Information such as diagnosis in the example below, will be pre-populated in the screen.
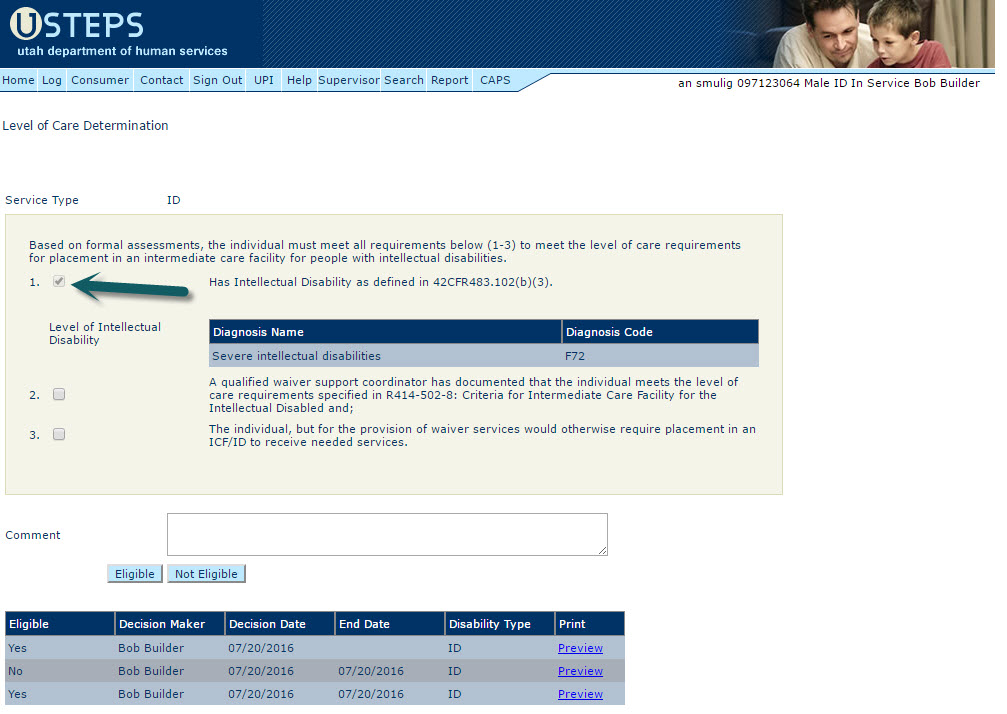
To establish that a person meets the Level of Care, the remaining check boxes must be selected and the Eligibility button must be clicked.
A message indicating your "Decision has been recorded" will be displayed at the top of the screen and the Level of Care decision will then be recorded in the table at the bottom of the page:
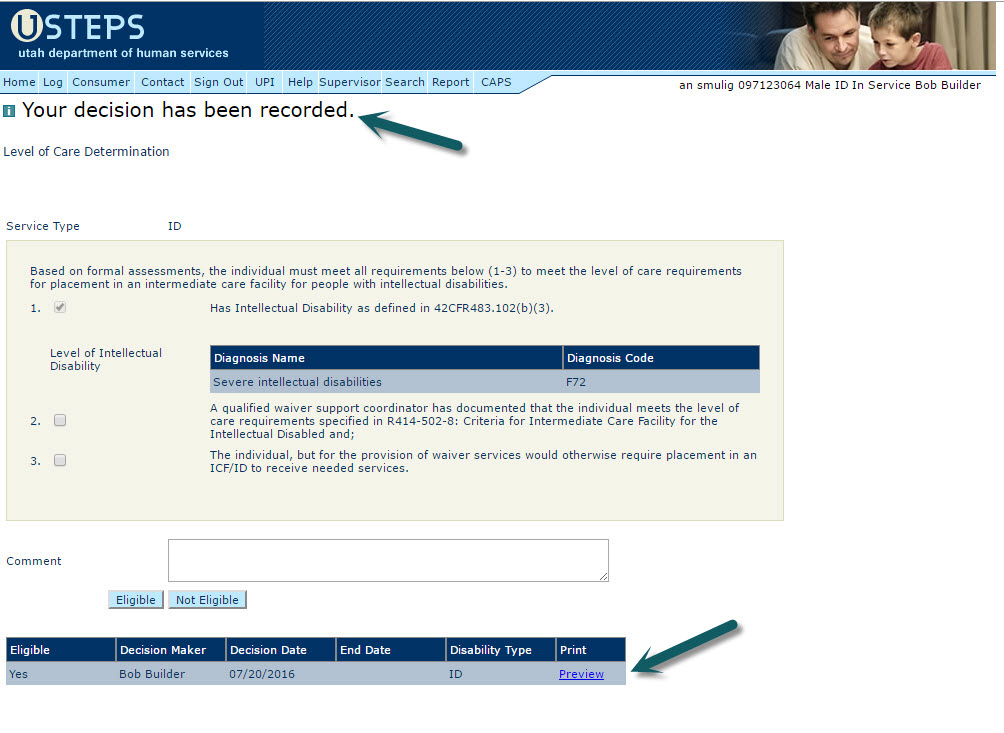
Please note: Level of Care Eligibility must be documented at least every 12-months for People who are In-Services.
Once DSPD has established that the Person in services meets the Level of Care, the Person must make application to the Bureau of Eligibility Services in the Department of Workforce Services to assess the meeting of Financial requirements for Medicaid. DSPD facilitates this application and documents the results of the application in the USTEPS system.
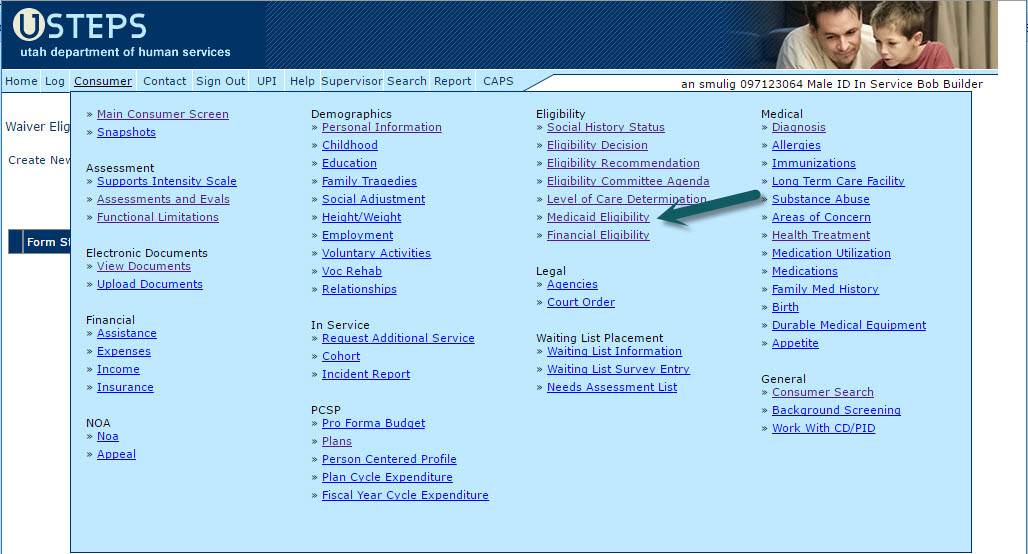
To request and document the Medicaid Financial eligibility, begin by selecting the Medicaid Eligibility screen in USTEPS:
The Medicaid Form 927, request for Financial Eligibility determination is a 3 part process. Part 1 of the form is completed and printed from the USTEPS system. The USTEPS system utilizes data that has been previously entered into USTEPS. When completed and printed, Part 1 is sent to DWS and is a request for financial eligibility determination. Part 2 is the response from DWS. When part 2 is received, the information from the form is entered into USTEPS to document the outcome of the request. The final Part 3, is completed and printed when the Person is being disenrolled from the Home and Community Based Waiver program.
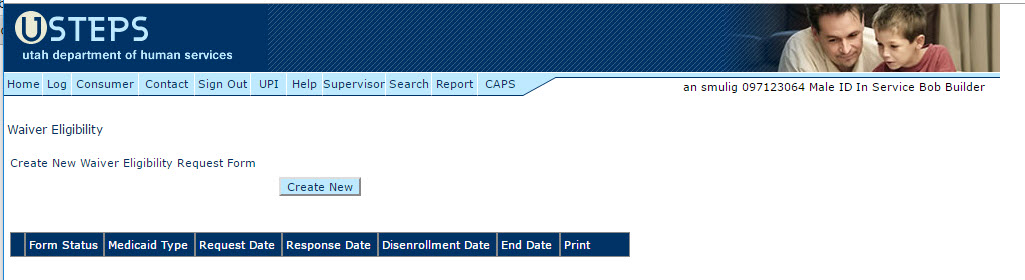
Completing Part 1. The user simply clicks on the "Create New" button on the Medicaid Waiver Eligibility page. The waiver eligibility page also has a history of financial eligibility requests in table form. If the Person has an open waiver eligibility request, the "Create New" option will not be available.
Once the "Create New" button has been clicked, the user will be taken to Part 1 of the Form 927. This section is automatically completed with information previously entered into USTEPS. The user will only need to click the "Submit Request to DWS/Print" option. The Form 927 will download to allow printing.
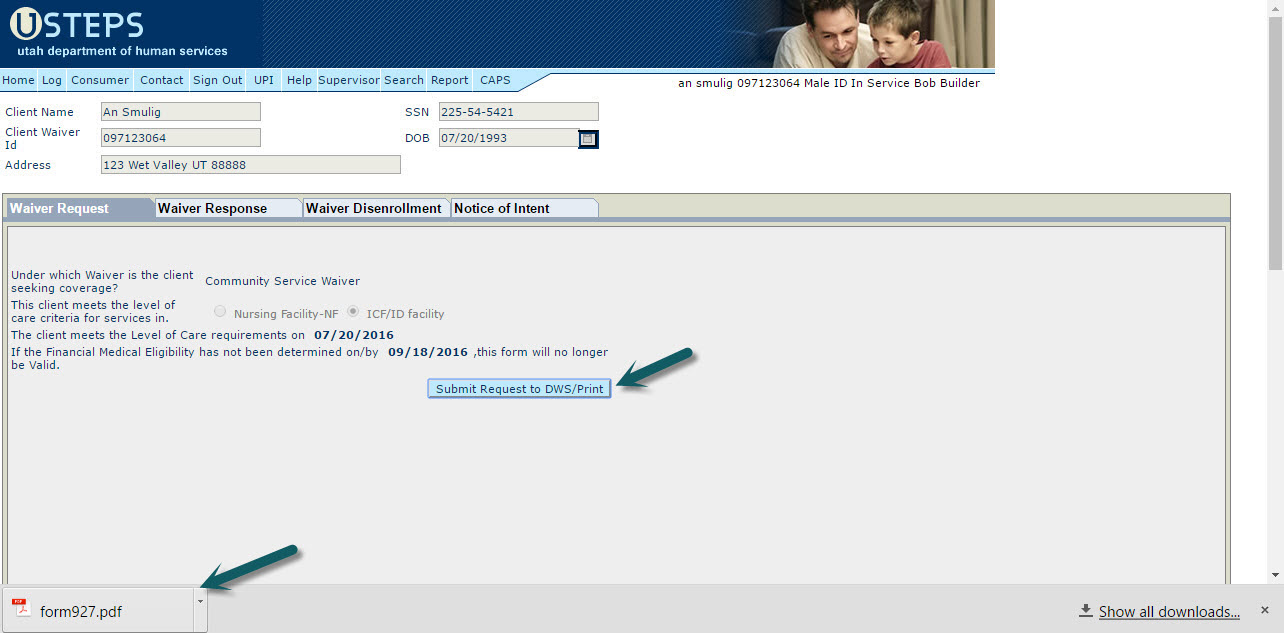
Please note: The form927.pdf download process will be dependent on the browser that you are using and may not be displayed as in the above example.
The Form 927 with Part 1 completed is scanned and e-mailed to the Bureau of Eligibility Services in the Department of Workforce Services.
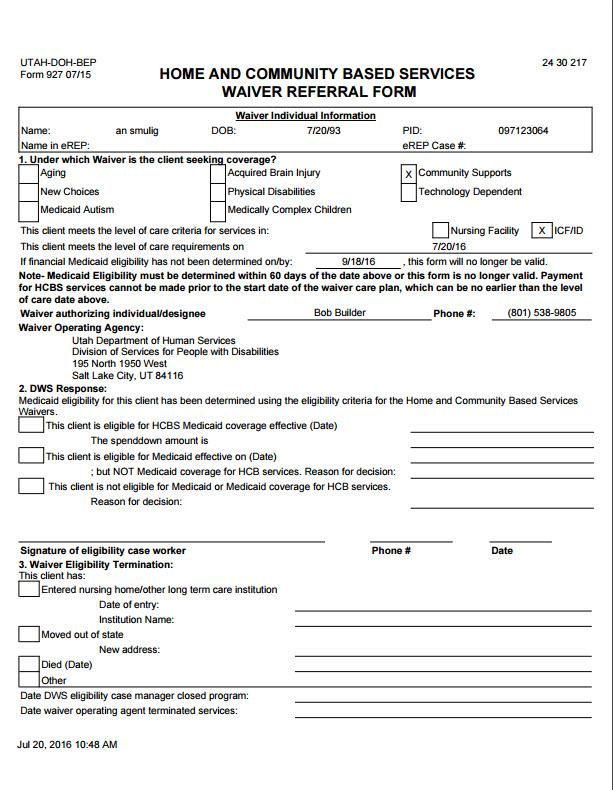
Example of a Form 927 with Part 1 completed:
When the Form 927 is returned from DWS, the response data is entered into USTEPS. The Medicaid request is selected from the data table and will open up for the user. The user selects the "Waiver Response" tab.
The Form 927 Part 2 screen will display the required information based upon the finding of "Eligible" or "Not Eligible".
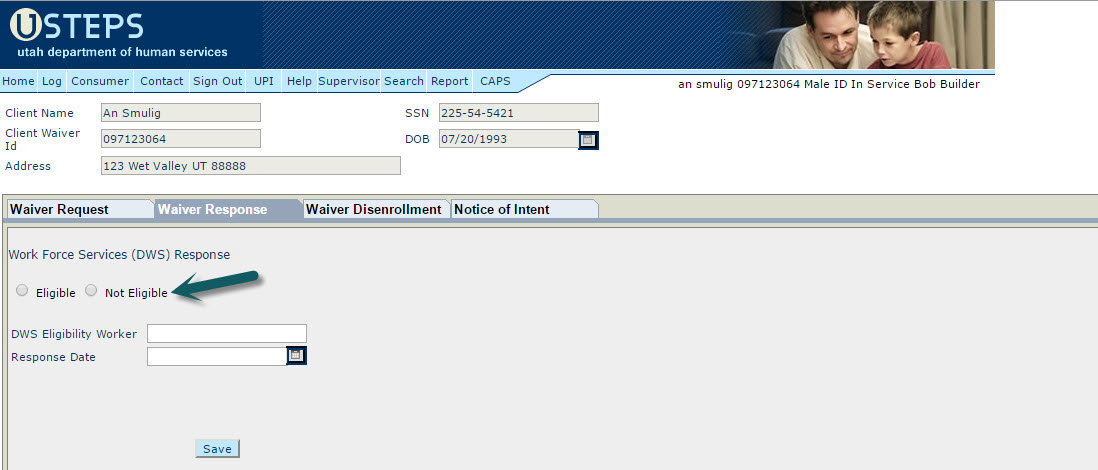
The following example demonstrates the information for a Person who is financially eligible for a "HCB Medicaid" waiver. Once the data has been entered, the user clicks the "Save" button and the data will be stored in the USTEPS system.
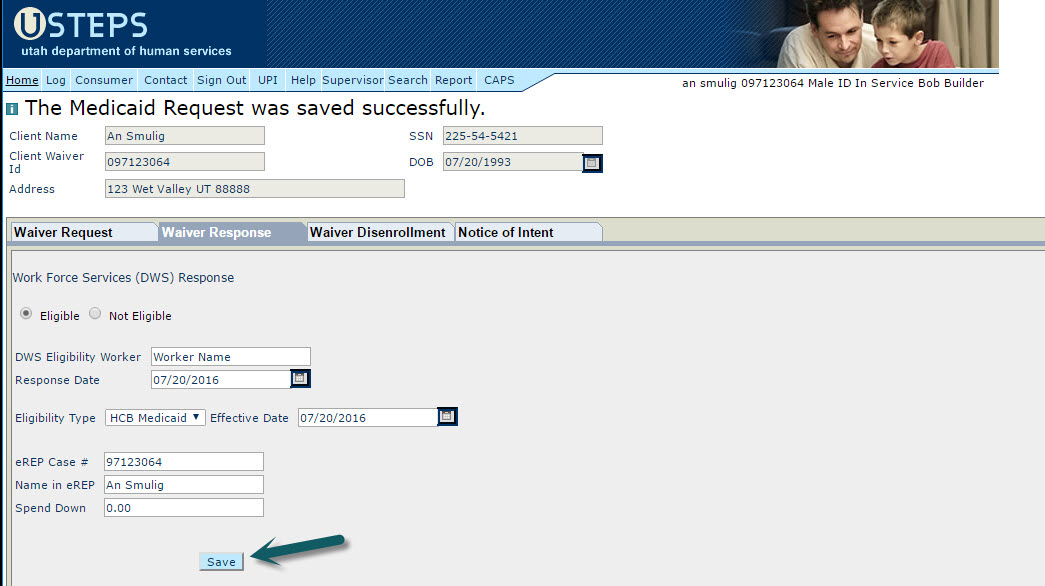
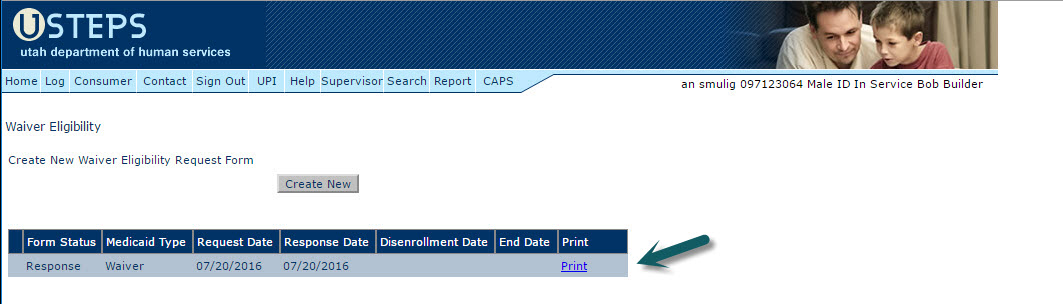
The data table on the "Medicaid Eligibility" screen will be updated based on the data that was entered.
The waiver status on the form 927 does not need to be updated unless there is a change of status. However, as noted above, the Level of Care determination is required to be updated every 12-months. DWS will review the financial eligibility on a monthly basis. In the event that the Level of Care is not met, or the Financial Eligibility is no longer met, the DSPD eligibility worker will need to begin the process of completing Part 3 to dis-enroll the Person from the HCBS waiver.
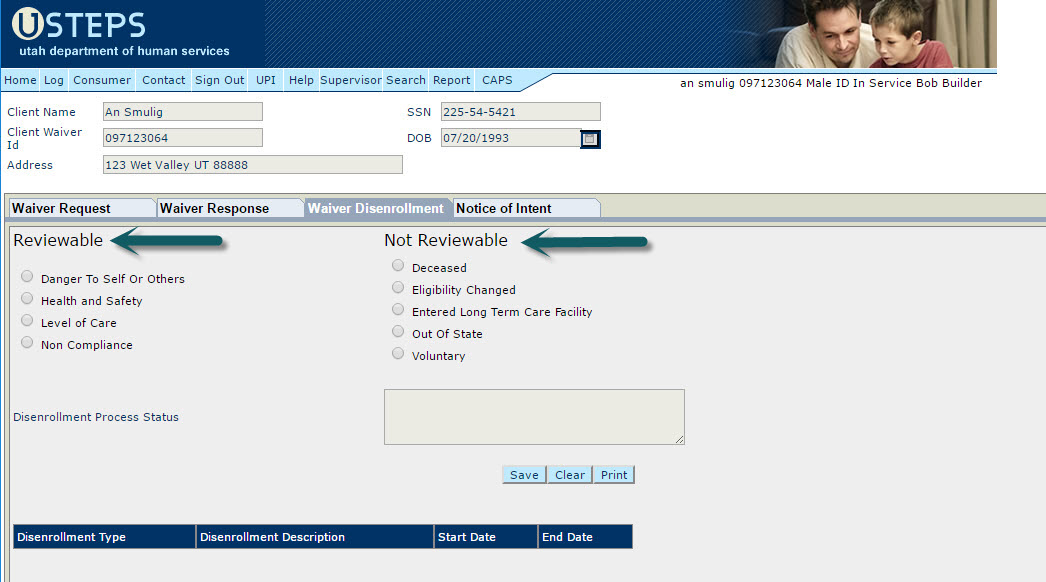
Dis-enrolling a Person from the HCBS waiver falls into one of two types: "reviewable" or "non-reviewable". The Waiver Disenrollment tab lists the valid categories for each
type of dis- enrollment.
When Dis-enrolling a person for a "Non-Reviewable" reason, select the reason and click the "Save" button. Once the "Save" button is clicked you will need to enter the dis-enrollment date and click the "Save" button a second time. The dis-enrollment will now be finalized.

The Medicaid Eligibility table will be updated with the dis-enrollment.

Reviewable Waiver Dis-enrollments must be approved by the Bureau of Authorization and Community-Based Services (BACBS) in the Department of Health.
The "Reviewable" dis-enrollment reasons are listed on the Waiver Dis-enrollment tab. When selecting a "Reviewable" reason, a "Notice of Intent" must be submitted to and approved by the BACBS in the Department of Health. To begin the Reviewable dis-enrollment, the user selects the reason and clicks "Save".
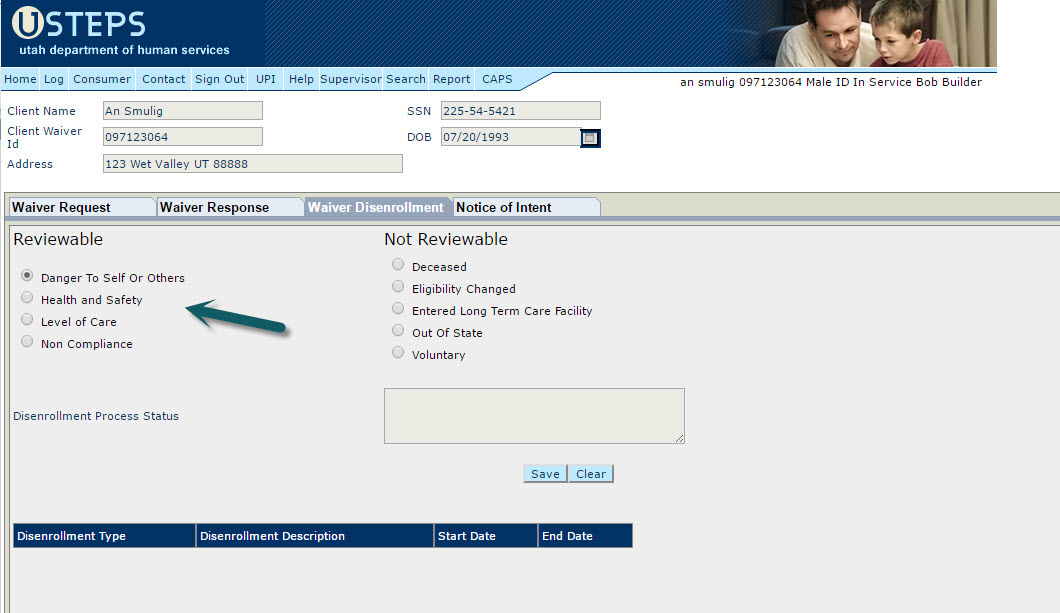
Once the reason has been saved, the user proceeds to the "Notice of Intent" tab.
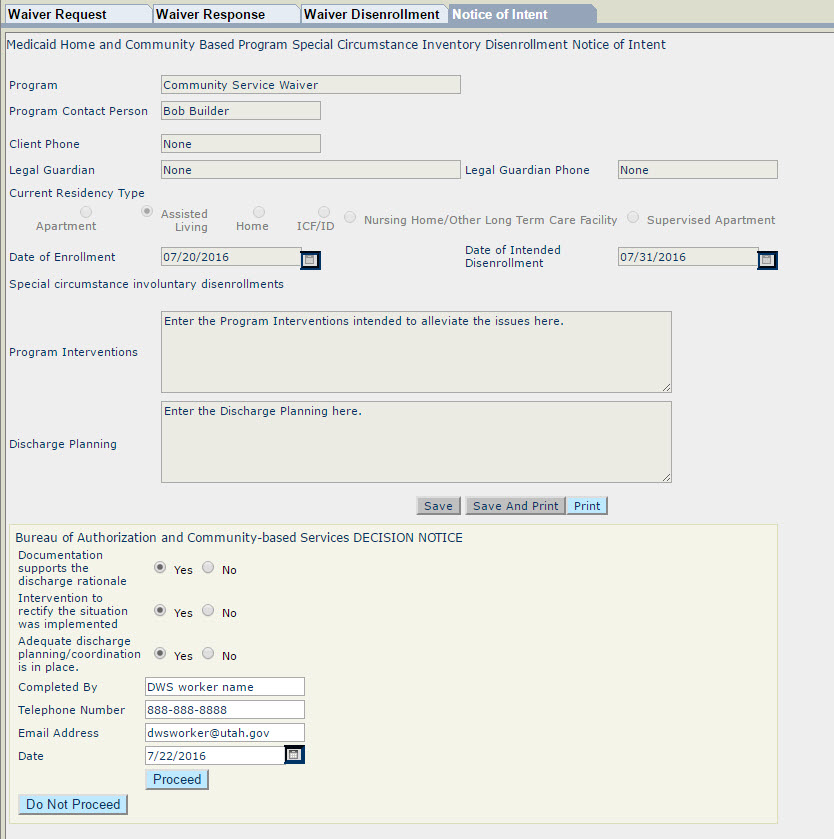
The Notice of Intent will have much of the information auto-populated. The use will need to complete sections as indicated in the example below:
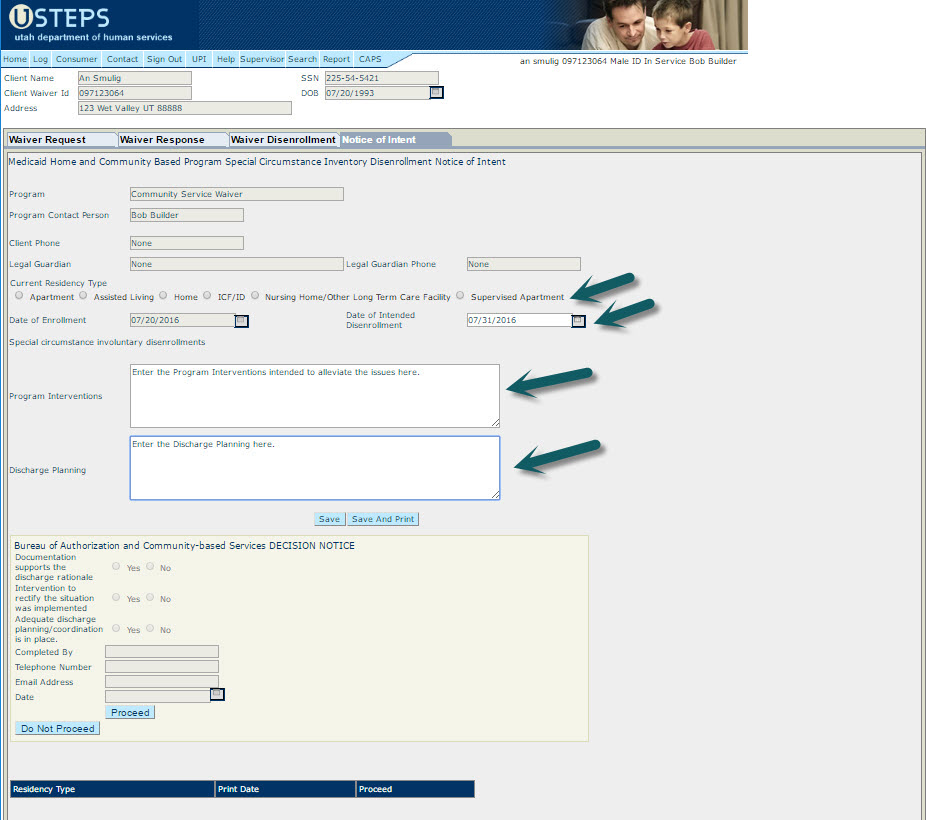
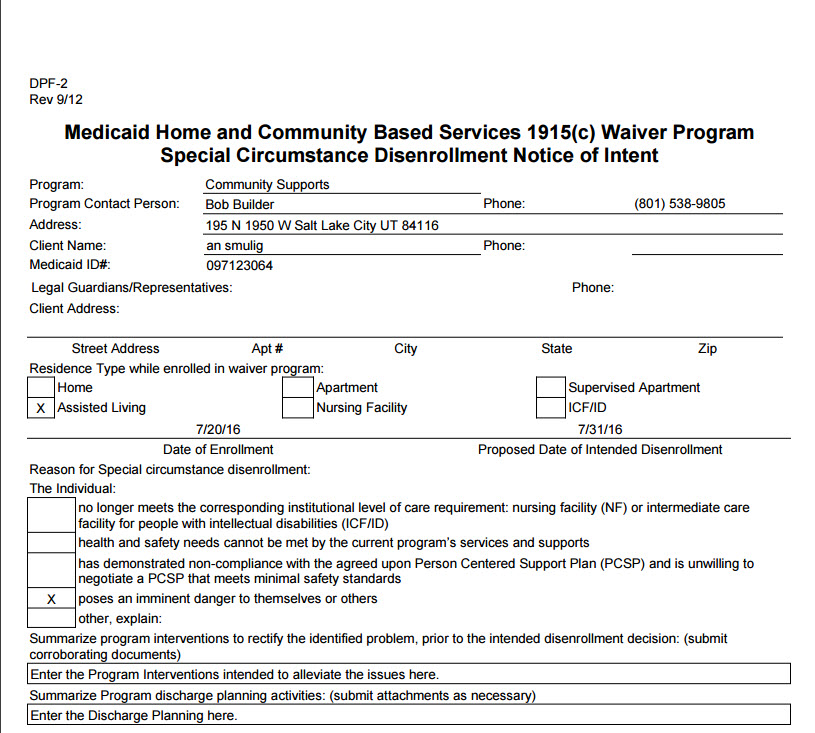
Once the information is completed, the form can be saved and printed ("Save and Print" button). The printed form is sent to the BACBS in the Department of Health.
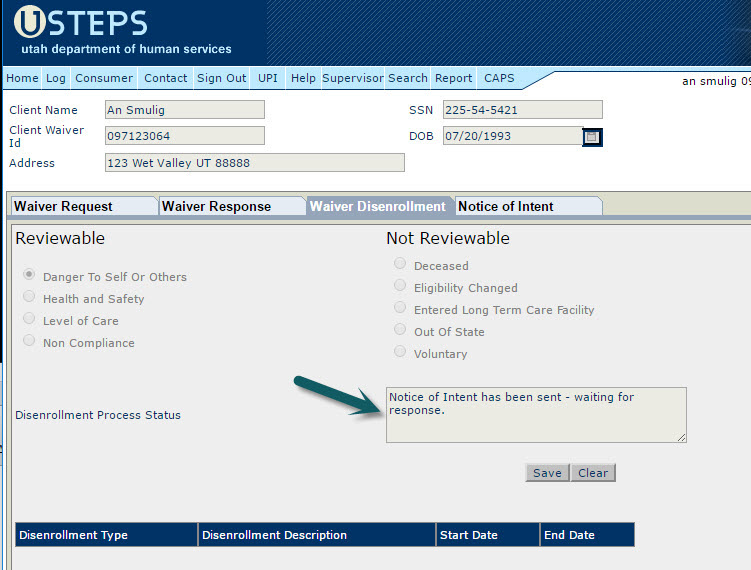
The Dis-enrollment Status on the Waiver Dis-enrollment is updated tab once the form has been printed.
BACBS will complete and return the Notice of Intent:
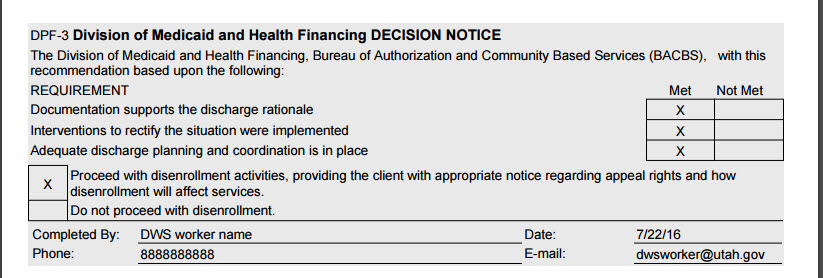
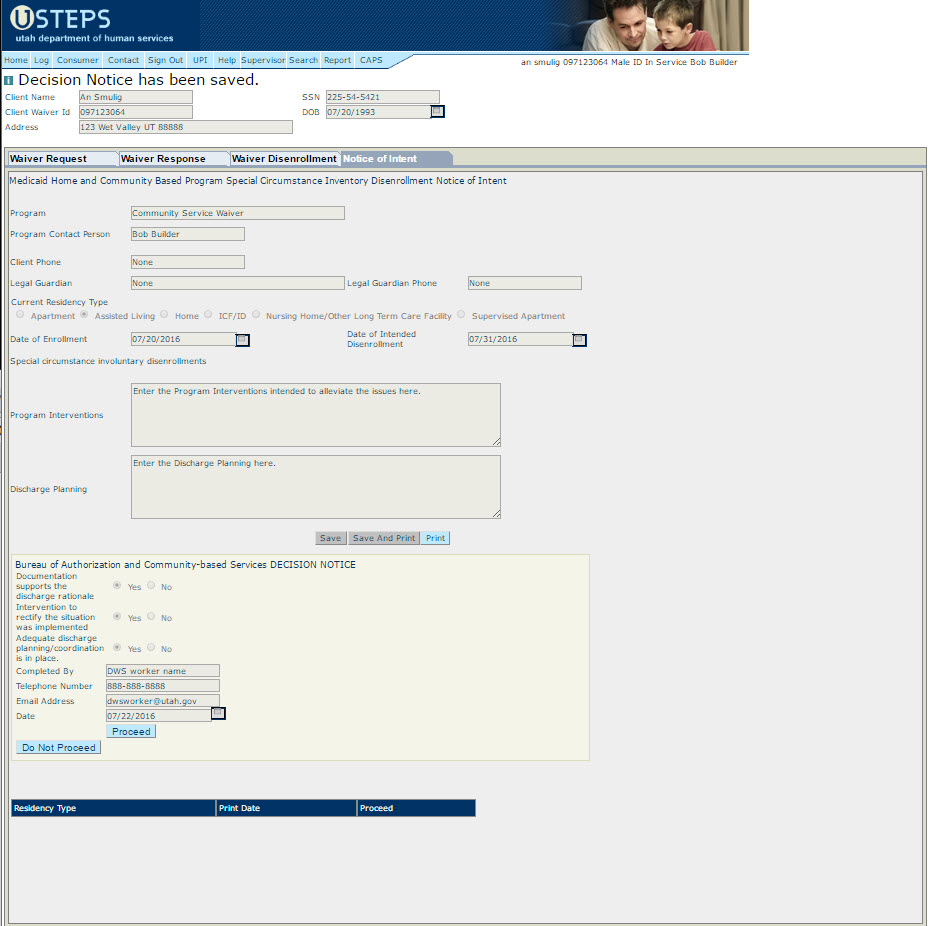
When the response is returned, the information is entered on the "Notice of Intent" screen and saved. In the following example, the disenrollment was approved. The user enters the information and selects "Proceed".
When the information has been entered, and Proceed has been selected, a confirmation message will be displayed at the top of the screen.
If BACBS confirms the decision to disenroll the Person from the HCBS waiver, DSPD proceeds to either terminate the Person from all services or to change the services to the State funding only.
If BACBS dos not allow DSPD to proceed, the person stays (or returns) to the HCBS waiver with no changes to their service funding level.